Discrimination increases the risk for negative cardiovascular health outcomes, according to a new study led by Quynh Nguyen in the University of Maryland School of Public Health. While many recent scientific studies point to a link between being chronically exposed to racial discrimination and poor health, this new research, published in the Journal of Racial and Ethnic Health Disparities, went beyond what people say they are experiencing and used social media data to characterize racism in the broader social environment.
“We’re trying to capture what may be invisible, but still affects people’s lives,” said Nguyen, an assistant professor of epidemiology. “Using Twitter data allows us to look at not just people’s individual experiences of discrimination, but the broader context of the social environment. Understanding area-level characteristics gives us a broader way of characterizing and examining the influence of discrimination on health.”
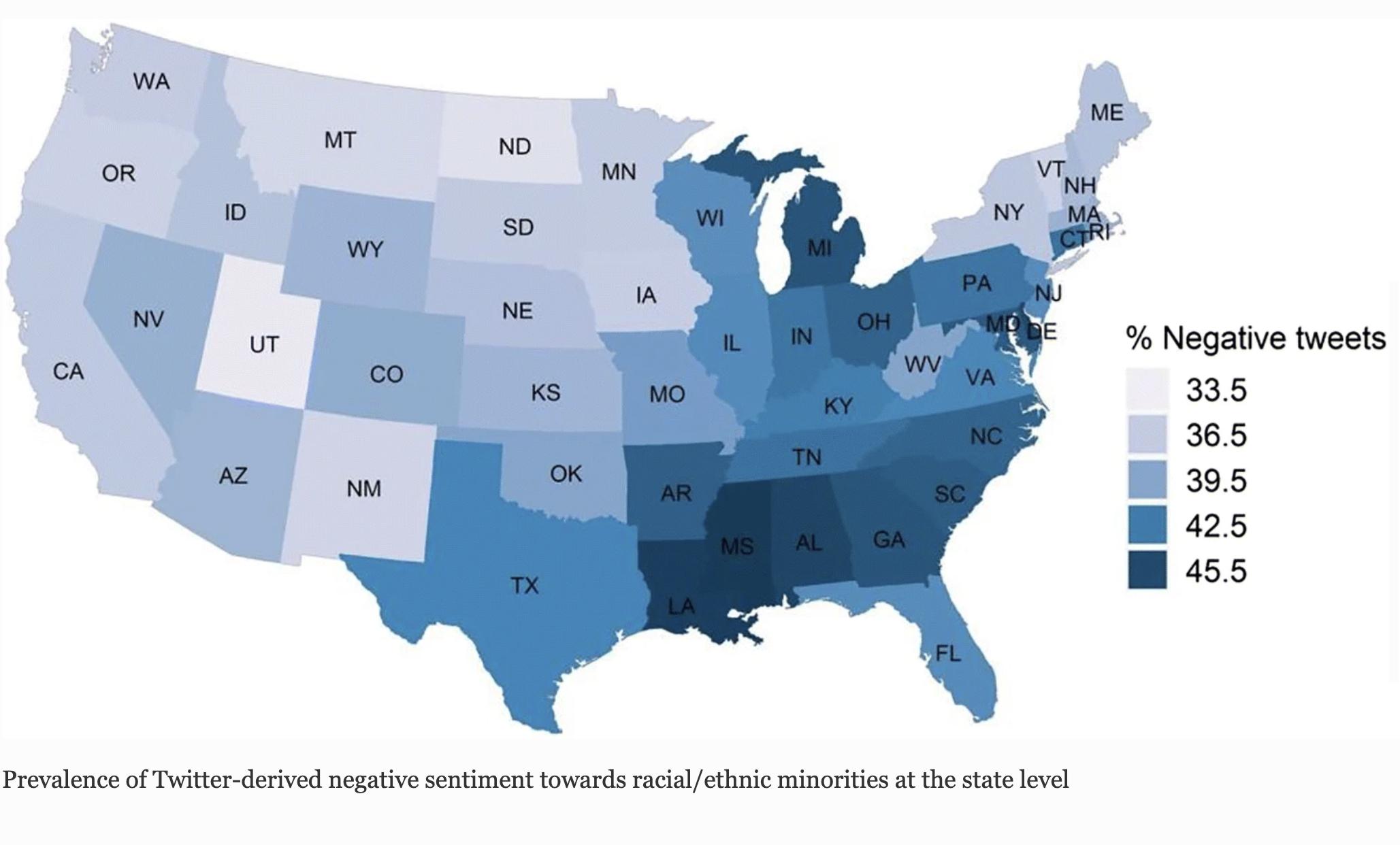
Nguyen and colleagues collected a 1% random sample of tweets using Twitter Streaming Application Programming Interface (API) across 48 states in the contiguous USA and the District of Columbia. Using big data methods, they categorized more than 30 million race-related tweets over a three year period (2015 to 2018) by positive, negative or neutral sentiments and by state. They linked the state-by-state tweet data with cardiovascular disease risk factors reported through the telephone-based survey Behavioral Risk Factor Surveillance System conducted annually by the Centers for Disease Control and Prevention.
Those living in states from which the highest number of racist tweets originated - including Mississippi, Louisiana and Michigan - had a higher prevalence of high blood pressure (+11%), diabetes (+15%), obesity (+14%), stroke (+30%), heart attacks (+14%) and other cardiovascular disease outcomes. Those living in states from which there were tweets with more positive sentiments towards racial and ethnic minorities - including Utah, North Dakota and California - had a lower prevalence of cardiovascular disease.
These poorer health outcomes were seen in both non-Hispanic Blacks and non-Hispanic whites.
“A lot of the past research has focused only on associations between adverse outcomes and discrimination among minorities, so this finding that adverse outcomes are seen among whites as well is new. Although whites are not the recipients of discrimination against minorities, racial hostility may still behave like a stressor and be linked with worse outcomes. A social environment characterized by more negativity may be bad for population health overall,” Nguyen explained.
Related Links: