
Poster # 38
Title: Pediatric patients with sickle cell disease in South Carolina: a descriptive study, 2002-2018
Presenting Author: Melissa DeSantiago MPH (doctoral student Johns Hopkins SPH)
Co-Authors: Lesliam Quiros Alcala, JHU, affiliate faculty UMD SPH, Varada Shevade, Geographical Sciences, BSOS, Robin Puett, MIEH, SPH
Faculty Mentors: Robin Puett
Primary Category: Health Equity, Racism and Social Injustice, Population Health, Immigration and Health
Secondary Category: Research on Health Disparities, in Memory of Mitchell Stewart
Background: Identifying demographic and socioeconomic disparities and trends in hospital admissions of pediatric patients with sickle cell disease will provide valuable information to better target public health educational campaigns and improve access to care.
Goals: We sought to to examine acute health care utilization during an 18-year period (2002-2019) for pediatric patients with sickle cell disease in South Carolina
Objectives: We hypothesize that there will be differences in hospitalizations over time, by sex, age, payor, rural/urban residential area and comorbidities.
Approach/Methods: We used 18 years of administrative data for pediatric SCD hospital admissions from January 1, 2002 through December 31, 2019 and conducted epidemiologic descriptive statistics.
Results: Hospital encounters were highest among the youngest age group, suggestion of gender differences, higher proportion of patients in rural areas living below federal poverty level.
Importance to public health: Advances in preventive care and new medicines have reduced the life-threatening problems of SCD; however, it is still a chronic and sometimes fatal disease, therefore proper surveillance is critical for better prognosis and to identify the needs and barriers for seeking adequate care.
Poster # 39
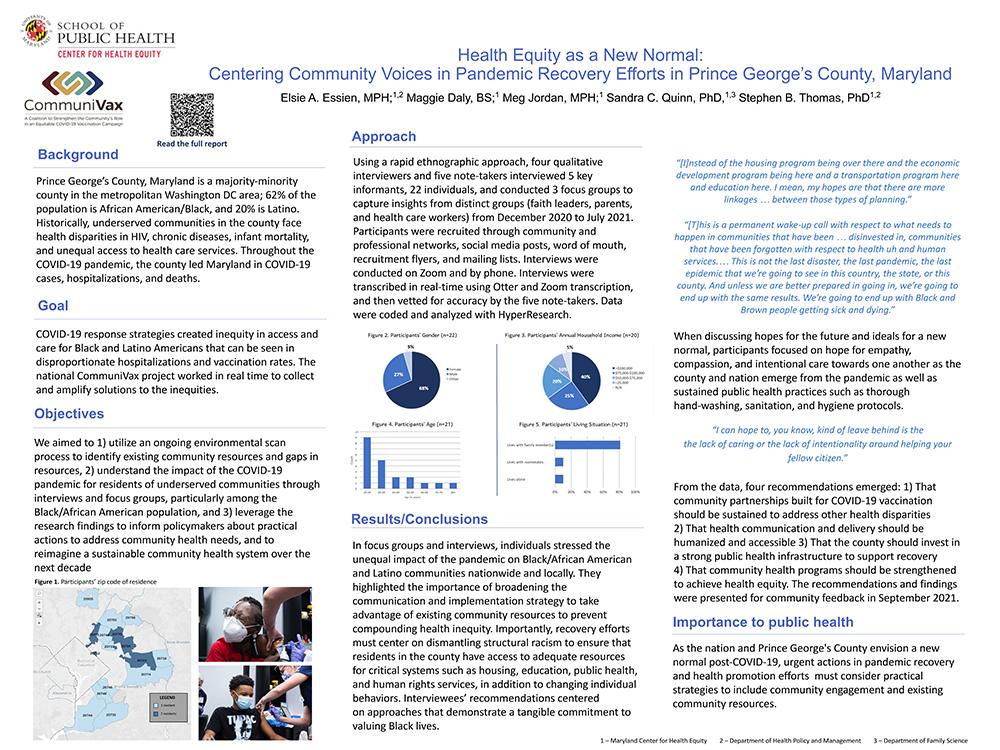
Title: Health Equity As a New Normal: Centering Community Voices in Pandemic Recovery Efforts in Prince George's County, Maryland
Presenting Author: Elsie Essien (doctoral student UMD SPH Health Policy and Management)
Authors: Maggie Daly, BS; Project Manager; Maryland Center for Health Equity, Meg Jordan, MPH; Project Coordinator; Maryland Center for Health Equity, Sandra C Quinn, PhD; Professor and Chair, Department of Family Science; Senior Associate Director, Maryland Center for Health Equity, Stephen B Thomas, PhD; Professor, Health Policy & Management; Director, Maryland Center for Health Equity
Faculty Mentors: Stephen B Thomas, PhD; Sandra C Quinn, PhD
Primary Category: Healthy Equity, Racism and Social Injustice, Population Health, Immigration and Health
Secondary Category: COVID-19
Background: Historically, underserved communities in Prince George's County, Maryland, face health disparities and unequal access to health care services. Throughout the COVID-19 pandemic, the county led Maryland in COVID-19 cases, hospitalizations, and death.
Goals: COVID-19 response strategies created inequity in access and care for Black and Latino Americans that can be seen in disproportionate hospitalizations and vaccination rates. The national CommuniVax project worked in real time to collect and amplify solutions to the inequities.
Objectives: We aimed to 1) utilize an ongoing environmental scan process to identify existing community resources and gaps in resources, 2) understand the impact of the COVID-19 pandemic for residents of underserved communities through interviews and focus groups, particularly among the Black/African American population, and 3) leverage the research findings to inform policymakers about practical actions to address community health needs, and to reimagine a community health campaign sustainable over the next decade.
Approach/Methods: Using a rapid ethnographic approach, four qualitative interviewers and five note-takers interviewed 5 key informants, 22 individuals, and conducted 3 focus groups to capture insights from distinct groups (faith leaders, parents, and health care workers) from December 2020 to July 2021. Participants were recruited through community and professional networks, social media posts, word of mouth, recruitment flyers, and mailing lists. Interviews were conducted on Zoom and by phone. Interviews were transcribed in real-time using Otter and Zoom transcription, and then vetted for accuracy by the five note-takers. Data were coded and analyzed with HyperResearch.
Results: In focus groups and interviews, individuals stressed the unequal impact of the pandemic on Black/African American and Latino communities nationwide and locally. They highlighted the importance of broadening the communication and implementation strategy to take advantage of existing community resources and crucial to prevent compounding health inequity. Importantly, recovery efforts must center on dismantling structural racism to ensure that residents in the county have access to adequate resources for critical systems such as housing, education, public health, and human rights services, in addition to changing individual behaviors. Interviewees’ recommendations centered on approaches that demonstrate a tangible commitment to valuing Black lives. When discussing hopes for the future and ideals for a new normal, participants focused on hope for empathy, compassion, and intentional care towards one another as the county and nation emerge from the pandemic as well as sustaining good public health practices such as continued hand-washing, sanitation, and hygiene protocols.
Importance to public health: As the nation and Prince George's County envision a new normal post-COVID-19, urgent actions in pandemic recovery efforts must consider practical strategies to include community engagement and existing community resources.
Poster #40
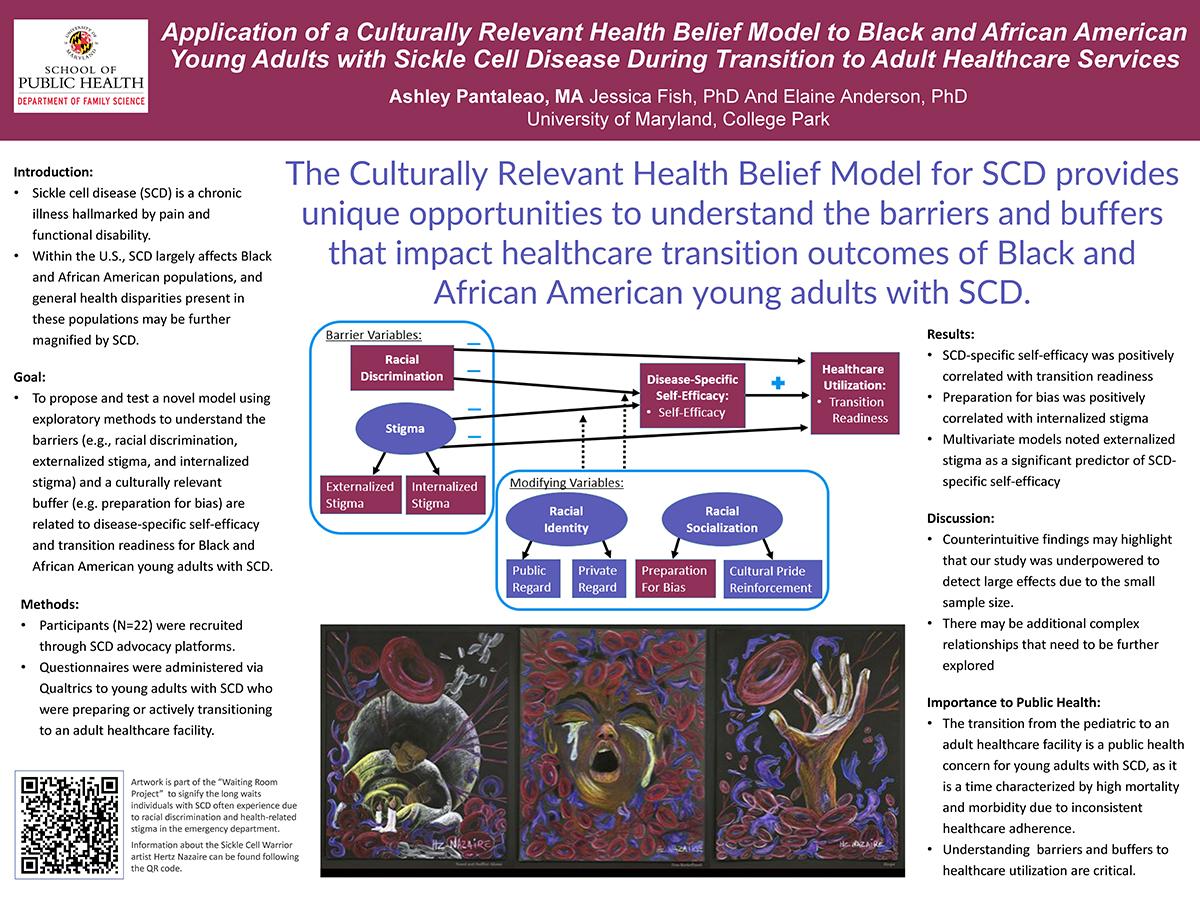
Title: Application of a Culturally Relevant Health Belief Model to Black and African American Young Adults with Sickle Cell Disease During Transition to Adult Healthcare Services
Presenting Author: Ashley Pantaleao (UMD SPH Family Science doctoral student )
Authors: Jessica Fish; School of Public Health, Department of Family Science, University of Maryland, College Park; Faculty, Elaine Anderson; School of Public Health, Department of Family Science, University of Maryland, College Park; Professor Emerita
Faculty Mentors: Jessica Fish and Elaine Anderson
Primary Category: Healthy Equity, Racism and Social Injustice, Population Health, Immigration and Health
Secondary Category: Health Care, Access to Care, Insurance, Technology
Background: Sickle cell disease (SCD) is a chronic illness hallmarked by pain and functional disability that impacts psychosocial well-being. Within the U.S., SCD largely affects Black and African American populations, and general health disparities present in these populations may be further magnified by SCD.
Goals: A short-term goal was to highlight the value of identifying youth with high levels of perceived barriers to guide educational resources and interventions to increase self-efficacy and readiness to transition for this underserved illness group.
Objectives: This research assessed whether the perceived barriers (e.g., racial discrimination, externalized stigma, and internalized stigma) will be linked to SCD-specific self-efficacy and transitioning to the adult healthcare setting utilizing an adapted Health Belief Model. It additionally explored whether a culturally relevant factor, preparation for bias, contributes to transition readiness. This work was a first step in exploring the relationships between these variables utilizing the Culturally Relevant Health Belief Model.
Approach/Methods: Participants (N=22) were recruited through SCD advocacy platforms. Questionnaires were administered to young adults with SCD who were preparing for transition or actively transitioning to an adult healthcare facility.
Results: Strong positive significant correlations among perceived barrier variables were noted as well as a positive significant correlation between SCD-specific self-efficacy and transition readiness. Additionally, preparation for bias was correlated with transition readiness. Results from multivariate models suggest that externalized stigma was significantly positively related to SCD-specific self-efficacy. Counter to expectations, no significant predictors of transition readiness were identified. Additionally, results did not support preparation for bias moderating the relationships between racial discrimination or externalized stigma with SCD-specific self-efficacy or transition readiness. These findings may highlight that our study was underpowered to detect large effects, or that there are additional complex relationships that need to be further explored.
Importance to public health: The transition from the pediatric to an adult healthcare facility is a public health concern for young adults with SCD, as it is a time characterized by high mortality and morbidity due to inconsistent healthcare. Unexplored factors that may impact illness course and outcomes include health-related stigma, racial discrimination, and preparation for bias.
Poster #41
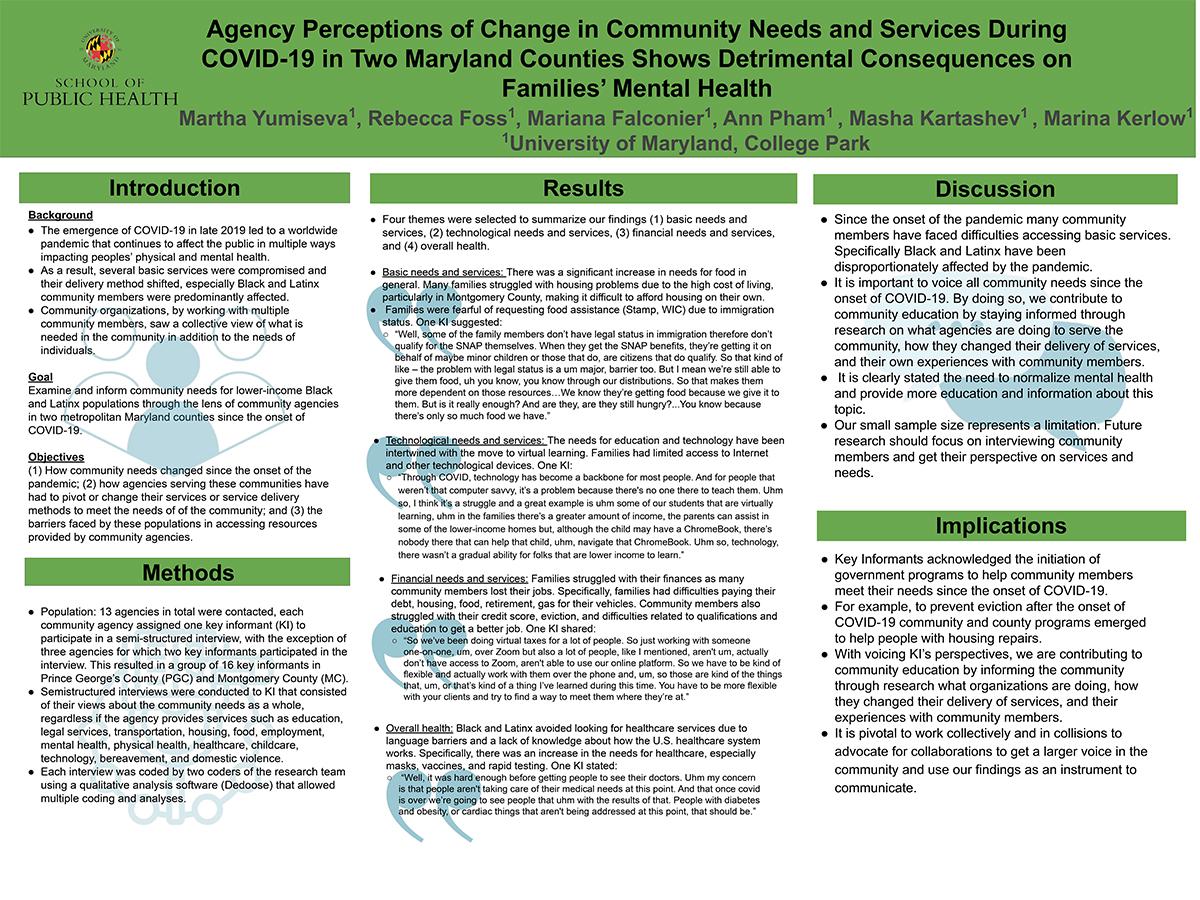
Title: Agency Perceptions of Change in Community Needs and Services During COVID-19 in Two Maryland Counties Shows Detrimental Consequences on Families’ Mental Health
Presenting Author: Martha Yumiseva (UMD SPH Family Science doctoral student )
Authors: Rebecca Foss, Family Science; Student, Mariana Falconier, Family Science, Faculty, Ann Pham, Family Science; Student, Masha Kartashev, Family Science; Student, Marina Kerlow; Family Science; Student
Faculty Mentors: Mariana Falconier
Primary Category: Healthy Equity, Racism and Social Injustice, Population Health, Immigration and Health
Secondary Category: COVID-19
Background: The emergence of COVID-19 in late 2019 led to a worldwide pandemic that continues to affect the public in multiple ways impacting peoples’ physical and mental health. Many Black and Latinx have struggled with access to technology, loss of employment and income added to the increase in household food insecurity, housing-related hardships, and accessibility to health insurance. Community organizations, by working with multiple community members, saw a collective view of what is needed in the community in addition to the needs of individuals.
Goals: Examine and inform community needs for lower-income Black and Latinx populations through the lens of community agencies in two metropolitan Maryland counties since the onset of COVID-19.
Background: The emergence of COVID-19 in late 2019 led to a worldwide pandemic that continues to affect the public in multiple ways impacting peoples’ physical and mental health. Many Black and Latinx have struggled with access to technology, loss of employment and income added to the increase in household food insecurity, housing-related hardships, and accessibility to health insurance. Community organizations, by working with multiple community members, saw a collective view of what is needed in the community in addition to the needs of individuals.
Goals: Examine and inform community needs for lower-income Black and Latinx populations through the lens of community agencies in two metropolitan Maryland counties since the onset of COVID-19.
Objectives: How community needs changed since the onset of the pandemic; (2) how agencies serving these communities have had to pivot or change their services or service delivery methods to meet the needs of of the community; and (3) the barriers faced by these populations in accessing resources provided by community agencies.
Approach/Methods: Semistructured interviews were conducted to KI that consisted of their views about the community needs as a whole, regardless if the agency provides services such as education, legal services, transportation, housing, food, employment, mental health, physical health, healthcare, childcare, technology, bereavement, and domestic violence.
Results: Four themes were selected to summarize our findings; (1) basic needs and services, (2) technological needs and services, (3) financial needs and services, and (4) overall health. Since the onset of the pandemic there was a significant increase in needs for food in general, the needs for education and technology have been intertwined with the move to virtual learning, families struggled with their finances as many individuals lost their jobs, and many Black and Latinx avoided looking for healthcare services due to language barriers and a lack of knowledge about how the U.S. healthcare system works. Because of loss of employment, people lost a lot of benefits and accessibility to care for themselves and their families.
Importance to public health: This study generates recommendations of best practices from community outreach during COVID-19 to safeguard the mental health of community members and voice the need to reinforce policies in mental health access for everybody.
